Allogeneic Stem Cell Transplantation for Relapsed and/or Refractory Hodgkin Lymphoma: A Multicenter Real World Experience
Introduction
Relapsed and/or refractory (R/R) Hodgkin Lymphoma (HL) after autologous stem cell transplant (SCT) is associated with poor outcomes and nearly 50% of patients will ultimately relapse. Novel therapeutic agents such as checkpoint inhibitors (CPIs) (nivolumab, pembrolizumab) and brentuximab vedotin (BV) have both shown considerable activity in this patient population, but allogeneic SCT (alloSCT) maintains its curative potential also in the era of new drugs. Herein we report on our multicenter experience with alloSCT for R/R HL.
Methods
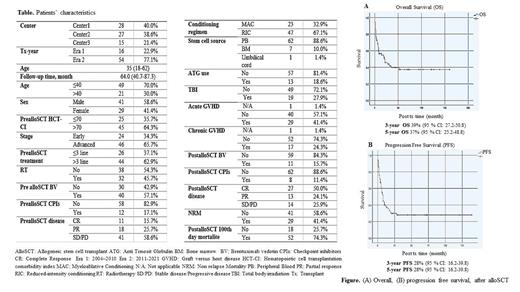
Seventy patients with R/R classic HL who underwent alloSCT between 2004 and 2021 in three transplant centers were included. Patients were included between 2004-2010 (era1) in one centre, 2011-2021 (era2) in all centers. Disease response was evaluated according to Lugano classification. Primary end point was post transplant (tx) overall response rate (ORR). Secondary endpoints were overall survival (OS), progression free survival (PFS), non relapse mortality (NRM) and response rates according to parameters especially tx years, and pre/post tx CPIs and/or BV usage.
Results
Patient characteristics are summarized in the Table. Median follow up time after alloSCT was 64 months (range, 40.7-87.3). Post tx disease relapse or progression occurred in 23 patients (33%). The median time to disease relapse was 6.3 months (range, 1-24.5). Twenty nine patients were alive at the analytic date (41%); 23 in complete response (CR) (79%), 4 partial response (PR) (14%), 2 stabl disease (SD) (7%). The 3-year OS, PFS were 39% (95% CI 27.2-50.8) and 28% (95% CI 16.2-39.8), respectively; the day 100 and 1-year NRM rates were 26% (95% 16.2-35.8) and 37% (95% CI 25.2- 48.8), respectively.
According to the tx year, the pre tx response rates were not statistically different between the two eras (p=0.46) but post tx CR rates were significantly higher in era2 (p=0.01). The survival (OS, PFS) analysis and NRM rates demonstrated no difference between both eras, but the PFS was significantly longer in 2016 and after (p=0.03). Patients who received alloSCT between era 1 and era 2 in one and only centre; the survival rates, and NRM were similar across the two eras.
The patients with chemosensitive disease (CR, PR) at the time of alloSCT had more common pre tx BV usage (p=0.03), RIC conditioning regimen (p=0.002), and were with high HCT CI score (p=0.02), while the low proportion of ATG usage (p=0.02). Achievement of a CR at pre tx associated with better OS, PFS, and NRM. Patients in CR at the time of the post tx was associated with significantly improved OS and PFS (p<0.05).
Patients who received BV and CPIs at any point pre and post tx had better OS, PFS and the NRM was low, but not statistically significant. There was a lower NRM rates in the post tx BV (p=0.06) and CPIs (p=0.08) usage.
Regarding to post tx cyclophosphamide (cy) versus ATG usage; patients who received ATG had signicantly shorter OS (p=0.04), an increase in NRM (p=0.01), but similar PFS (p=0.28) compared with those who did not. Patients who received post tx cy had signicantly better OS (p=0.04) and PFS (p=0.05) but similar NRM (p=0.19) compared with those who did not. There was no statistically significant difference in OS, PFS and NRM with regard to the conditioning regimens (RIC and MAC) (p>0.05).
Regarding donor type; the use of pre tx CPIs, TBI in conditioning regimen, and post cy were common for haploidentical (haplo) tx (p<0.05). ATG was used more commonly for matched/mismatched unrelated donor (MUD/MMUD) when compared with matched related donor (MRD) (p<0.001). The incidence of acute graft versus host disease (GVHD) (p=0.09) and chronic GVHD (p=0.002) were higher in patients who received MRD grafts when compared with MUD/MMUD and haplo. Haplo donors had significant better OS (p=0.015) and PFS (p=0.03) compared with MUD/MMUD and MRD. There was a significantly higher NRM in the MUD/MMUD compared with others (p<0.05).
Conclusions
Our results suggest that alloSCT continues to play an important therapeutic role for patients with R/R cHL. The improved outcomes of alloSCT in HL over time, probably due to general improvements in supportive care, a better selection of patients and the arrival of novel therapeutic therapies. The efficacy of alloSCT can be determined by multicenter prospective studies in selected patient groups.
Disclosures
Beksac:Takeda: Speakers Bureau; Sanofi: Speakers Bureau; Menarini: Membership on an entity's Board of Directors or advisory committees; BMS: Speakers Bureau; Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal